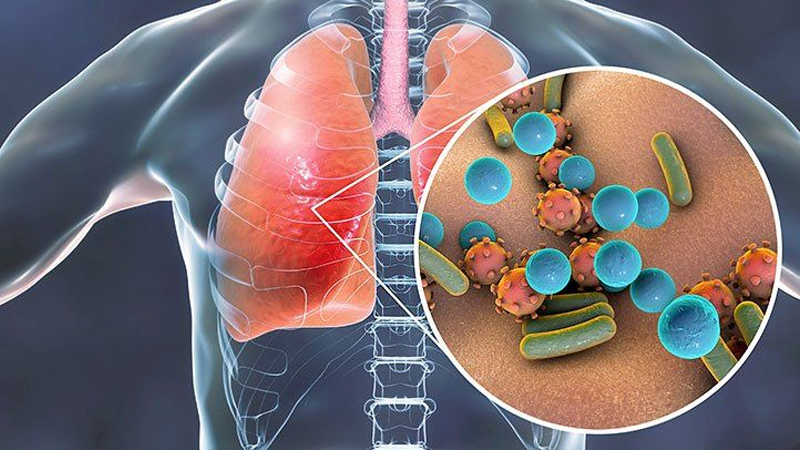
What is Tuberculosis (TB):
- A person contracts tuberculosis (TB) by breathing in microscopic droplets from an infected person’s cough or sneeze.
- Although it mostly affects the lungs, it can also have an impact on the stomach (abdomen), glands, bones, and nervous system.
- Although TB is a potentially serious infection, it is curable when treated with the appropriate drugs.
- To read about Tuberculosis Diagnosis click here
World Tuberculosis Day:
- Every year, World Tuberculosis Day is celebrated on March 24 to raise awareness about tuberculosis.

How Tuberculosis (TB ) Spread:
- The TB bacterium can be transferred from person to person through the air.
- Tuberculosis bacteria can enter the air when a person who has TB disease of the lungs or throat coughs, speaks, or sings.
- People nearby could inhale these microorganisms and acquire an infection.
- The TB bacteria can enter the lungs and start to develop there after being inhaled.
- They can then travel through the blood to the kidney, spine, and brain, among other organs.
- TB infection in the throat or lungs might be contagious.
- This implies that the bacteria can spread to more individuals.
- TB in other body parts, such the kidney or spine, is typically not contagious.
- The most likely recipients of TB infection from those who have it are those with whom they interact often.
- This includes family members, close friends, and coworkers or classmates.
Tuberculosis (TB) is not spread by?
- shaking hands
- sharing food or beverages
- touching toilet seats or bed sheets
- exchanging toothbrushes
- kissing
Tuberculosis Preventions:
- You will be infectious if you have pulmonary tuberculosis for up to two to three weeks after starting treatment.
- While you typically won’t need to be separated during this period, it’s still crucial to follow a few simple safety measures to prevent the spread of TB to your loved ones.
General measure for this are:
- Stay away from work, school, or college until your TB treatment team says it’s safe for you to return.
- Stay away from work, school, or college until your TB treatment team says it’s safe for you to return.
- Always cover your mouth when you cough, sneeze, or laugh. Carefully dispose of any used tissues in a sealed plastic bag.
- Open windows when you can to ensure that the spaces where you spend time have a sufficient supply of fresh air.
- Avoid sharing a bed with anyone else because you might sneeze or cough when you’re asleep
- To read about Tuberculosis Risk Factors click here
Tuberculosis Symptoms:
Typical symptoms of TB include:
- A cough that lasts longer than three weeks and frequently produces sputum, sometime which may be bloody
- Losing the weight
- Night sweats
- A fever
- Exhaustion, lack of energy,
- Appetite loss
- Neck swellings
- If your cough lasts longer than three weeks or you cough up blood, you should visit your medical professional.
Tuberculosis Bacteria:
Tuberculosis (TB) is a bacterial infection.
- Mycobacterium tuberculosis is a type of bacteria that causes tuberculosis (TB).

- The most contagious form of TB, known as pulmonary TB, normally only spreads after prolonged contact with an infected person.
- In the majority of healthy individuals, the immune system, the body’s natural defense against infection and disease, destroys the bacteria and there are no symptoms.
- Even when the immune system is unable to eradicate the bacteria, it can sometimes stop it from spreading throughout the body.
- Although you won’t experience any symptoms, the germs will still be present in your body, this term is is referred as Latent TB. Latent tuberculosis patients are not contagious.
- The infection can spread to the lungs or other parts of the body if the immune system is unable to eradicate it or keep it under control, and symptoms will appear within a few weeks or months. Active TB is what this is.
- Later on, latent TB could become active TB disease, especially if your immune system declines.
- When a person with active TB disease in their lungs coughs or sneezes, TB bacteria-containing droplets that are ejected are inhaled by the other person.
- Although TB spreads similarly to the flu or the common cold, it is not as contagious.
- To become infected oneself, you would need to come into intimate contact with an infected individual for a prolonged time (several hours).
- For instance, TB infections typically spread among members of the same family who reside in the same home. It would be extremely unlikely for you to contract the disease by sharing a seat, say, on a bus or train, with an affected person.
- Not all TB patients are contagious. People who have extrapulmonary TB (outside the lungs) or children who have TB do not spread the infection.
Types of Tuberculosis (TB):
A TB bacteria infection does not always result in illness. As a result, there are two TB-related conditions given below;
- Latent TB infection
- TB disease.
Latent TB Infection:
You can have TB infection in your body without any symptoms & without getting sick. It’s known as a latent TB infection. Most often, when TB bacteria are inhaled and an infection results, the body is able to resist the bacteria and prevent it from spreading.
People with Latent TB infection sufferers:
- Do not exhibit any symptoms;
- Do not feel ill;
- Cannot transmit the TB bacteria to others;
- Usually exhibit a positive skin test result or positive blood test for TB;
If they do not receive treatment for latent TB infection, they may develop TB Disease. Many persons with latent TB infection never experience the symptoms of TB disease. These people have inactive TB bacteria for the rest of their lives without developing any disease. However, in some individuals, particularly those with weakened immune systems, the bacteria become active, grow, and result in TB disease.
To read Latent Tuberculosis Diagnosis click here
Tuberculosis Disease:
- If the immune system is unable to prevent the growth of the TB bacteria, they become active.
- TB disease is a condition where the TB bacteria are active and multiplying within your body.
- Those who have TB disease are ill, and show TB disease symptoms.
- They could be able to pass the bacterium to those who they interact with frequently.
- Many persons with latent TB infection never experience the symptoms of TB disease.
- Some patients become ill with TB disease shortly after contracting the infection (within a few weeks), before their immune system has a chance to stop the TB bacteria.
- Others may contract a disease years down the road if their immune system deteriorates for some other cause.
- The chance of contracting TB disease is significantly higher for those with compromised immune systems, especially for those who are HIV-positive than for those with healthy immune systems.
- To read about Diagnosis of Tuberculosis Disease click here
The Difference between Latent TB Infection (LTBI) and TB Disease:
| Latent TB Infection (LTBI) | Tuberculosis disease. |
| no symptoms | symptoms that may include a bad cough that lasts 3 weeks or longer, pain in the chest, coughing up blood or sputum, weakness or fatigue, weight loss, no appetite, chills, fever & sweating at night |
| Does not feel sick | Usually feels sick |
| Cannot spread TB bacteria to others | May spread TB bacteria to others |
| Usually has a skin test or blood test result indicating TB infection | Usually has a skin test or blood test result indicating TB infection
|
| Has a normal chest x-ray and a negative sputum smear | May have an abnormal chest x-ray, or positive sputum smear or culture |
| Needs treatment for latent TB infection to prevent TB disease | Needs treatment to treat TB disease |
Two most common term are also describe Tuberculosis types, including;
Pulmonary Tuberculosis (PTB):
- A bacterial infection that affects the lungs is known as pulmonary tuberculosis (PTB). It might disperse to other organs.
- To read Pulmonary Tuberculosis Diagnosis click here
Extrapulmonary Tuberculosis (EPTB):
- The term “EPTB” describes TB that affects organs other the lungs (e.g., pleura, lymph nodes, abdomen, genitourinary tract, skin, joints and bones, or meninges). A person is said to have PTB if they have both pulmonary and EPTB.
- To read Diagnosis of Extrapulmonary Disease click here
What is Drug Resistant Tuberculosis?
- Bacteria that cause TB can occasionally develop resistance to the medications used to treat it. This indicates that the medicine is no longer effective in killing the TB germs.
- Drug-susceptible TB (DS TB) and drug-resistant TB (DR TB) both spread through the same mechanisms. TB is transferred from one person to another through the air.
- A person who has TB disease of the lungs or throat coughs, sneezes, speaks, or sings, releasing the TB bacteria into the air. Nearby individuals may inhale these microorganisms and acquire an infection.
How Drug Resistant Tuberculosis Spread?
Drug-resistant tuberculosis can occasionally develop when bacteria are treated with medications ineffectively or improperly. Misuse or poor management examples include:
- People don’t always finish the entire TB treatment regimen.
- The improper treatment is recommended by healthcare professionals (the wrong dose or length of time)
- There are no medications available for effective treatment.
- The standard of drugs is low.
- Drug-resistant tuberculosis is more typical among those who
- Do not routinely take their TB medications.
- Take only some of their TB medications.
- after receiving treatment for TB disease, contract the disease once again
- come from regions where drug-resistant TB is prevalent
- have interacted with a person who has drug-resistant tuberculosis
Types of Drug Resistant Tuberculosis?
Multidrug Resistant Tuberculosis (MDR TB):
- Multidrug-Resistant Tuberculosis (MDR TB) is brought about by TB germs that are at least resistant to the two most effective TB medications, isoniazid and rifampin. All people with TB illness are treated with these medications.
- When treating MDR TB, specialists in the disease should be consulted.
Pre-Extensively Drug Resistant Tuberculosis (pre-XDR TB):
- Pre-Extensively Drug-resistant tuberculosis (pre-XDR-TB) is a type of MDR-TB caused by TB bacteria that are resistant to fluroquinolone, isoniazid and rifampin OR by TB bacteria that are resistant to rifampin, isoniazid and a second-line injectable (amikacin, capreomycin, and kanamycin).
Extensively Drug Resistant Tuberculosis (XDR-TB)
- Extensively drug-resistant Tuberculosis (XDR-TB) is a rare type of MDR-TB caused by TB bacteria that are resistant to fluroquinolone, isoniazid, rifampin and a second-line injectable (amikacin, capreomycin, and kanamycin) OR by TB bacteria that are resistant to isoniazid, rifampin, a fluroquinolone, and bedaquiline or linezolid.
- Patients are left with treatment alternatives that are significantly less effective since XDR TB is resistant to the most potent TB medications.
- People who have HIV infection or other illnesses that can compromise their immune systems should pay special attention to XDR-TB. Once infected, these individuals have a higher likelihood of contracting TB disease, which increases their risk of death from TB disease
- When treating XDR-TB, specialists in the disease should be consulted.
How to Prevent Drug Resistant Tuberculosis?
- The most crucial step in preventing the spread of drug-resistant TB is to take all TB medications exactly as directed by your doctor.
- There should be no missed doses or early treatment termination. When taking medication for TB disease, patients should communicate any difficulties with their doctor.
- By promptly detecting cases, according to advised treatment protocols, observing patients’ responses to treatment, and ensuring medication is finished, healthcare professionals can help prevent drug-resistant TB.
- Avoiding exposure to known drug-resistant TB patients in enclosed or congested settings, such as hospitals, jails, or homeless shelters, is another strategy to prevent contracting the disease.
- Consult infection control or occupational health specialists if you work in a hospital or other healthcare facility where TB patients are likely to be seen.

Pingback: What are the Tuberculosis diagnosis & Tuberculosis risk factors?
Pingback: Tuberculosis treatment of children, adults and pregnant women.