Tuberculosis Treatment:
- After the diagnosis of tuberculosis we move towards to tuberculosis treatments, which mainly involves, Tuberculosis Drugs (Mainly Antibiotics) and Tuberculosis Vaccine for Active Tuberculosis Disease.
- When left untreated, latent tuberculosis infection can swiftly turn into Active Tuberculosis Disease specially in HIV-positive individuals since their immune systems are already compromised. Additionally, TB disease has a fatal prognosis if untreated.
- People with HIV or without HIV, who simultaneously have latent TB infection or TB disease fortunately have a variety of therapeutic choices.
- The location of the TB germs in the body affects the symptoms of TB disease. Most often, TB germs develop in the lungs (pulmonary TB).
- Lung TB disease may manifest as symptoms such:
- chest pain
- an acrid cough lasting three weeks or longer
- coughing up blood or sputum (phlegm from deep inside the lungs)
Other symptoms of TB disease are
- weakness or exhaustion
- loss of weight
- Lack of appetite and chills
- fever
- Perspiring at night
- Symptoms of TB disease in other parts of the body depend on the affected areas.
People who have latent TB infection
- Are symptom-free and don’t feel any fever and chill
- show no signs of TB disease, and
- cannot transmit TB to others.
What is Latent & Active Tuberculosis?
- Most healthy individuals have an immune system that can eliminate the TB-causing germs.
- But occasionally, the bacteria invade the body but do not produce any symptoms (latent TB), or the infection takes weeks, months, or even years to produce symptoms (active TB).
- Years after the original infection, up to 10% of patients with latent TB eventually acquire active TB.
- This typically occurs within the first year or two of infection or when the immune system is compromised, such as when undergoing chemotherapy for cancer.
Pulmonary TB
- TB can almost always be cured with treatment. Typically, an antibiotic course must be taken for six months.
- Because some strains of TB are resistant to particular medications, a variety of antibiotics are required.
- Treatment with six or more different drugs may be necessary if you have TB and it is drug-resistant.
- If you have pulmonary tuberculosis, you will remain contagious for 2 to 3 weeks after starting therapy.
- While you typically won’t need to be separated during this period, it’s still crucial to follow a few simple safety measures to prevent the infection from spreading to your loved ones.
You should:
- cover your mouth when you cough, sneeze, or laugh;
- carefully dispose of any used tissues in a sealed plastic bag;
- open windows when possible to ensure a good supply of fresh air in the areas where you spend time;
- Avoid sleeping in the same room as others until your TB treatment team says it’s safe to do so.
- Refrain from going to work, school, or college until your TB treatment team says it’s okay for you to do so.
You might undergo testing to determine your infection status if you have been in close contact with someone who has TB. A chest X-ray, blood tests, and a skin test also known as the Mantoux test are a few examples of these.
Tuberculosis Drugs:
- Tuberculosis drugs mainly involve different kind of antibiotics but also includes some other preventive medications.
- Taking antibiotics for several months is typically part of the treatment for tuberculosis (TB).
- TB is a dangerous condition that can be fatal if ignored, but once treatment is completed, fatalities are uncommon.
- Most patients don’t require hospital admission during their care.
- If you are determined to have active pulmonary TB, where your lungs are impacted and you have symptoms, you will be given a prescription for at least a 6-month course of a combination of antibiotics.
- The typical course of treatment includes:
- Two antibiotics (isoniazid and rifampicin) for 6 months
- Two extra antibiotics (pyrazinamide and ethambutol) for the first 2 months of the treatment period of 6 months
- Before you start to feel better, it can take a few weeks. Your general health and the degree of your TB will determine the precise amount of time.
- The majority of patients feel better and are no longer contagious after taking antibiotics for two weeks.
- But it’s crucial to keep taking your medication exactly as directed and finish the entire antibiotic course.
- The most effective strategy to guarantee the TB bacteria are eliminated is to take treatment for six months.
- The TB infection may become resistant to the medications if you stop taking your antibiotics before finishing the course or miss a dosage.
- This has the potential to be dangerous since it may be challenging to treat and will require a lengthier course of care with several, potentially hazardous medicines.
- Your medical team can work with you to find a solution if you struggle to take your medication on a daily basis.
- This may entail maintaining regular touch with your treatment team at your home, the treatment facility, or another more convenient location.
- If the course of treatment is followed correctly, you shouldn’t require any additional examinations by a TB specialist. Though it’s uncommon, you might receive guidance on how to recognize symptoms of a recurrence of the condition.
Tuberculosis Vaccination:
- A vaccination for tuberculosis (TB) is called Bacille Calmette-Guérin (BCG). In the US, this vaccine is not frequently utilized. BCG does not always safeguard individuals from contracting TB.
- On the recommendations of NHS, the BCG vaccine is advised for infants, young children, and those under the age of 35 who are thought to be at risk of contracting TB since it offers protection against the disease.
- Anyone above the age of 35 is not typically administered the BCG vaccine because there is no proof that it is effective in this age group.

BCG Recommendations
- Only those who meet particular requirements and in consultation with a TB expert are given the option of receiving BCG in the United States.
- If medical professionals have any queries regarding BCG vaccination for their patients, they should contact their state’s or region’s TB control program.
BCG vaccine for TB is a best choice for followings;
- Children or young people residing in regions with high TB prevalence
- People who have close family members who come from countries with high TB rates.
- People who plan to spend more than three months living and working with locals in a region with high TB rates.
- No matter your age, if you work in healthcare institution come into contact with patients or clinical samples,
You should get vaccinated against tuberculosis (TB) if the following criteria are met;
- you haven’t had the shot before (you don’t have a BCG scar or the necessary paperwork)
- the results of a Mantoux skin test or TB interferon gamma release assay (IGRA) blood test are negative.
Children:
Getting vaccinated with BCG should only be an option for kids who have had a negative TB test and are regularly exposed, and can’t be separated from other family members who are;
- unable to receive long-term primary preventive treatment for TB infection due to untreated or inadequate TB disease
- Possess TB disease strains that are rifampin- and isoniazid-resistant.
Health Care Workers:
BCG vaccination for healthcare workers should be taken into consideration on a case-by-case basis in environments where:
- A high proportion of TB patients have drug-resistant TB strains that are resistant to both isoniazid and rifampin.
- There is ongoing transmission of drug-resistant TB strains to healthcare workers and subsequent infection is likely.
- Extensive TB infection-control measures have been put in place but have not been effective.
The hazards and advantages of both the BCG vaccine and the treatment of latent TB infection should be discussed with healthcare personnel who are considering becoming vaccinated against BCG.
Testing for TB in BCG-Vaccinated People:
- BCG vaccinations are common among those who were born outside of the United States.
- A tuberculosis skin test may be administered to people who have already received the BCG vaccine to check for TB infection.
- A BCG vaccination may result in a positive TB skin test outcome. A BCG vaccination or an infection with the TB bacteria may be to blame for a positive result on a TB skin test.
- Contrary to TB skin tests, TB blood tests (IGRAs) are unaffected by past BCG vaccination and are not anticipated to produce a false-positive result in BCG recipients.
- The TB skin test is favored over the TB blood test for children under the age of five.
- Only the presence of the TB bacterium is revealed by a positive TB skin test or TB blood test.
- It cannot determine whether a person has TB disease or a latent infection.
- To determine if the subject has TB, more examinations are required, such as a chest x-ray and a sputum sample.
Tuberculosis Treatment and Pregnancy:
- A pregnant mother and her foetus are more at risk from untreated tuberculosis (TB) than from its treatment. When TB is suspected, treatment should start as soon as possible.
- Although the medications used in the initial TB treatment regimen cross the placenta, they do not appear to have any negative effects on the baby.
- Infants born to women with untreated TB may have lower birth weights than infants born to women without TB, and in rare cases, the infant may be born with TB.
- To prevent giving unneeded medicine to pregnant women, therapy for latent TB infection can typically be postponed until 2-3 months after delivery.
- Treatment for latent TB infection should not be postponed due to pregnancy alone, even during the first trimester, for women who are at high risk for developing TB disease from a latent TB infection, particularly those who are recent contacts of someone with infectious TB disease.
Tuberculosis Treatment Regimens for Pregnant Women
| Diagnosis | Treatment |
|
Latent Tuberculosis Infection. |
|
Tuberculosis Disease. |
|
HIV & Tuberculosis Disease |
|
Contraindications
The following anti-tuberculosis medications should not be used by expectant mothers:
- Streptomycin
- Amikacin
- Kanamycin
- Capreomycin
- Fluoroquinolones
Drug-Resistant Tuberculosis:
Due to known and unknowable complications associated with second-line anti-tuberculosis medications, pregnant women receiving treatment for drug-resistant TB should get counselling regarding the risk to the foetus.
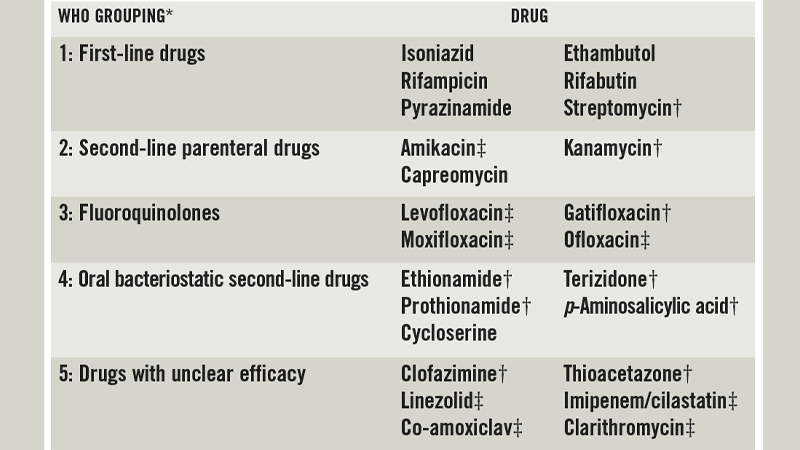
Treatment of Drug Resistant Tuberculosis:
- Drug Resistant Tuberculosis is caused by TB bacteria that are resistant to at least one of the first-line Anti-Tuberculosis drug. Multidrug-resistant Tuberculosis (MDR-TB) is resistant to more than one Anti-Tuberculosis drug and at least Isoniazid (INH) and Rifampin (RIF).
- Extensively drug-resistant Tuberculosis (XDR-TB) is a rare type of MDR-TB that is resistant to isoniazid and rifampin, plus any fluoroquinolone and at least one of three injectable second-line drugs (i.e., amikacin, kanamycin, or capreomycin).
- Drug Resistant Tuberculosis is challenging to treat and cure. Life threatening outcomes can result from poor management. A specialist in the disease should be consulted closely when managing drug resistant tuberculosis.
Fluoroquinolone Antibacterial Drug Safety Announcement:
- Due to potential side effects, the US Food and Drug Administration (FDA) has warned against using fluoroquinolone antibiotics to treat several straightforward illnesses.
- For example, the FDA stated that for patients with sinusitis, bronchitis, and uncomplicated urinary tract infections who have other treatment options, the risks of fluoroquinolone antibacterial medication side effects generally outweigh the benefits.
- Fluoroquinolone antibacterial drugs are absolutely necessary for some patients who have drug-resistant TB disease or drug-resistant latent TB infection or who cannot tolerate first-line TB drugs, although patients taking fluoroquinolone antibacterial drugs for tuberculosis (TB) also have a chance of experiencing the side effects noted by the FDA.
- Since TB is not a trivial infection but rather a potentially fatal or crippling disease, there are no better options available for these TB patients, and the advantages of fluoroquinolone antibacterial medications exceed the hazards.
- If you have any queries about fluoroquinolone antibacterial medications and you have TB, please get in touch with your doctor or the local or state TB control organisation.
- Please get in touch with your local or state TB control programme if you’re a medical professional and have inquiries about the use of fluoroquinolone antibacterial medications in TB therapy.
Breastfeeding:
- Because the amounts of these drugs in breast milk are too low to induce toxicity in the nursing newborn, breastfeeding should not be discouraged for mothers receiving the first-line anti-tuberculosis medications.
- Drugs in breast milk are ineffective in treating TB disease or latent TB infection in a nursing newborn for the same reason.
- Women who are breastfeeding and taking INH should also supplement with pyridoxine (vitamin B6). RIF may turn bodily fluids, especially breast milk, an orange color.
- Body fluids occasionally turning orange is normal and safe. The 3HP regimen may not be safe for women to use while nursing, according to the available research.
- Children are more susceptible than adults to contracting TB disease if exposed to the TB germs, and they also tend to deteriorate more quickly than adults.
- Compared to children, adults typically develop TB disease as a result of a prior TB infection that reactivates years later when the immune system of the patient becomes compromised for some reason (e.g., HIV infection, diabetes).
- In the management of newborns, young children, and children with immunodeficiencies who have been exposed to someone with infectious TB disease, a pediatric tuberculosis expert should be included.
- It is crucial that kids and anybody else receiving treatment for latent TB infection or TB disease follow the doctor’s instructions exactly and take the medication to completion.
Latent Tuberculosis Infection Treatment for Children:
- Children with latent TB infection should receive treatment to prevent them from getting the disease.
- Due to their higher risk of contracting the disease, infants, young children, immunocompromised kids, kids with latent TB infections, and kids who are in close proximity to those who have infectious TB disease, need special attention. Before starting treatment, it is suggested that you consult with a pediatric tuberculosis specialist.
- Latent TB infection can be treated in children older than 2 years old with once-weekly isoniazid-rifapentine treatments for a total of 12 weeks.
- Rifampin for four months daily or isoniazid for nine months daily are two alternative treatments for latent TB infection in children.
- The regimens are both acceptable, but doctors should, whenever possible, prescribe the shorter, more convenient regimens. Shorter treatment plans are more likely to be completed by patients.
Tuberculosis Disease Treatment for Children:
- Depending on the treatment protocol, TB disease in children is managed by taking a number of anti-TB medications for 4, 6, or 9 months.
- The 4-month rifapentine-moxifloxacin TB treatment combination is not advised by the CDC for kids under the age of 12 or who weigh less than 40 kilogram.
- A child runs the risk of getting sick again if they stop taking their medication before it’s finished.
- The germs that are still alive may develop treatment resistance if medications are not taken properly. Drug-resistant TB requires a longer, more difficult, and more expensive course of treatment (up to 18 to 24 months).